

This approach is cost‐effective and person‐centered and facilitates integrated care of co‐occurring mental and general medical disorders in individuals with SUDs. At lower levels of need, individuals can receive informal community care through support of friends and family or self‐help groups. At the next level, primary care health services can provide screening and brief interventions, referral to a specialist (when needed), and follow‐up of individuals who may no longer need higher‐intensity interventions. Greater need levels can benefit from outpatient or inpatient specialized treatment services.
We are not aware of any controlled trials of medications for alcohol use disorder in pregnant women. Substance use and SUDs increase the risk of HIV and HCV infections, accounting for approximately 10% of the former305 and 38‐79% of the latter306 globally. Injection of drugs also increases risk of bacterial endocarditis, cellulitis, and abscesses and embolisms of the heart, brain and spleen, among other infections307.
Just as humans need a physiological immune system to fight off disease and illness, likewise, the relational attachment system provides protection against psychological problems and illness. Without a healthy attachment system, a child is much more vulnerable to stress and therefore more susceptible to having problems with trauma, anxiety, depression, and other mental illness. Attachment theory posits that the quality of the parents’ attachment system that developed in infancy will affect their ability to form healthy attachments to their own children and with other adults. Substance use disorders involve a pathologic pattern of behaviors in which patients continue to use a substance despite experiencing significant problems related to its use.
For example, individuals can be diverted from the justice system at pre‐arrest and linked to clinical and social services, including harm reduction or case management. The distribution of sterile injecting equipment through syringe services programs is an effective intervention for preventing HIV and hepatitis C virus (HCV) infections261. These programs can also serve as sites for low‐barrier treatment of substance abuse262. The rate of transition from substance use to a SUD varies by the type of substance, based on its pharmacological properties148, 156, 157, availability, legality, and social acceptability156, 157. The cumulative rate of transition has been reported to be 16‐67.5% for nicotine use disorder, 14‐22.7% for alcohol use disorder, 17‐20.9% for cocaine use disorder, 23% for heroin use disorder, and 8.9% for cannabis use disorder148, 158. Comorbidities between psychiatric disorders and SUDs are also relevant to prevention efforts.
Overdose prevention is a critical element of efforts to prevent substance use disorders, particularly in the context of rising opioid-related mortality. Clinicians should educate patients and families about the risks of overdose, especially when opioids are prescribed, and co-prescribe or dispense naloxone (eg, intranasal naloxone/Narcan) to individuals at elevated risk. Equipping patients and communities with naloxone, along with instructions on its use, is an evidence-based harm-reduction strategy that saves lives and facilitates linkage to care.
Although active substance abuse can impair attachment and healthy modeling for affect regulation, sometimes the consequences of severe and ongoing substance abuse on the part of a parent can result in parent and child separation. In extreme cases, the separation may be due to the substance-related death of the parent from overdose, motor vehicle accident, or medical complications due to substance abuse. The significant increase in out-of-home child placements in the 1980s and 1990s closely paralleled the pandemic drug addiction in the United States during those decades (Jaudes & Edwo, 1997). Any long-term separation will have a negative impact on the child’s ability to attach, regulate affect, and can lead to a trauma response of numbing or hyperarousal (inability to discriminate and respond appropriately to stimulus).
Yet, individuals may start using or misusing substances, such as opioids, after their school years287. There is still a need for research to develop and test preventive interventions for people who are at increased risk of developing SUDs, especially substance use disorder young adults288. There is also a need to study the efficacy of after‐school activities (e.g., sports) and interventions targeting youth at increased risk273. Greater knowledge of the influence of media in the psychosocial development of young people and their risk for substance use is also needed. This communication contains certain “forward-looking statements” within the meaning of the U.S. federal securities laws.
Lastly, social workers play an essential role in specialized courts (family courts, mental health courts, adult drug courts, and juvenile drug courts), providing a unique person in environment and multisystems lens to helping children and families. Specialized drug courts have been shown to produce favorable outcomes for the whole family (Burns, Pullman, Weathers, Wirschem, & Murphy, 2012). Prevention of substance use disorders encompasses targeted and universal strategies aimed at mitigating risk factors and bolstering protective factors across developmental stages. In clinical practice, prevention efforts should begin early, particularly during adolescence, when initiation of substance use is most likely and neurobiological vulnerability to addiction is heightened. Implicit in this type of model is the integration of substance use services with services for other mental disorders as well as primary care.
Opioids are narcotic, painkilling drugs produced from opium or made synthetically. This class of drugs includes, among others, heroin, morphine, codeine, methadone, fentanyl and oxycodone. It is also efficacious in reinforcing non‐drug‐re lated behavior, such as adherence to medications for human immunodeficiency virus (HIV) infection and maintaining low HIV viral load238. It can be used at different points of the treatment sequence, including initial engagement167, attendance237, 239, and abstinence237, 239, 240.
Diagnosis of substance use disorder is based on identifying a pathologic pattern of behaviors in which patients continue to use a substance despite experiencing significant functional impairment related to its use. The DSM-5-TR classification is organized into 4 categories that include a total of 11 criteria. Individuals meeting 2 or more of these criteria within a 12-month period are considered to have a substance use disorder. There are a number of genetic and epigenetic factors, which vary by specific substance, that impact the likelihood of developing a substance use disorder and its progression.
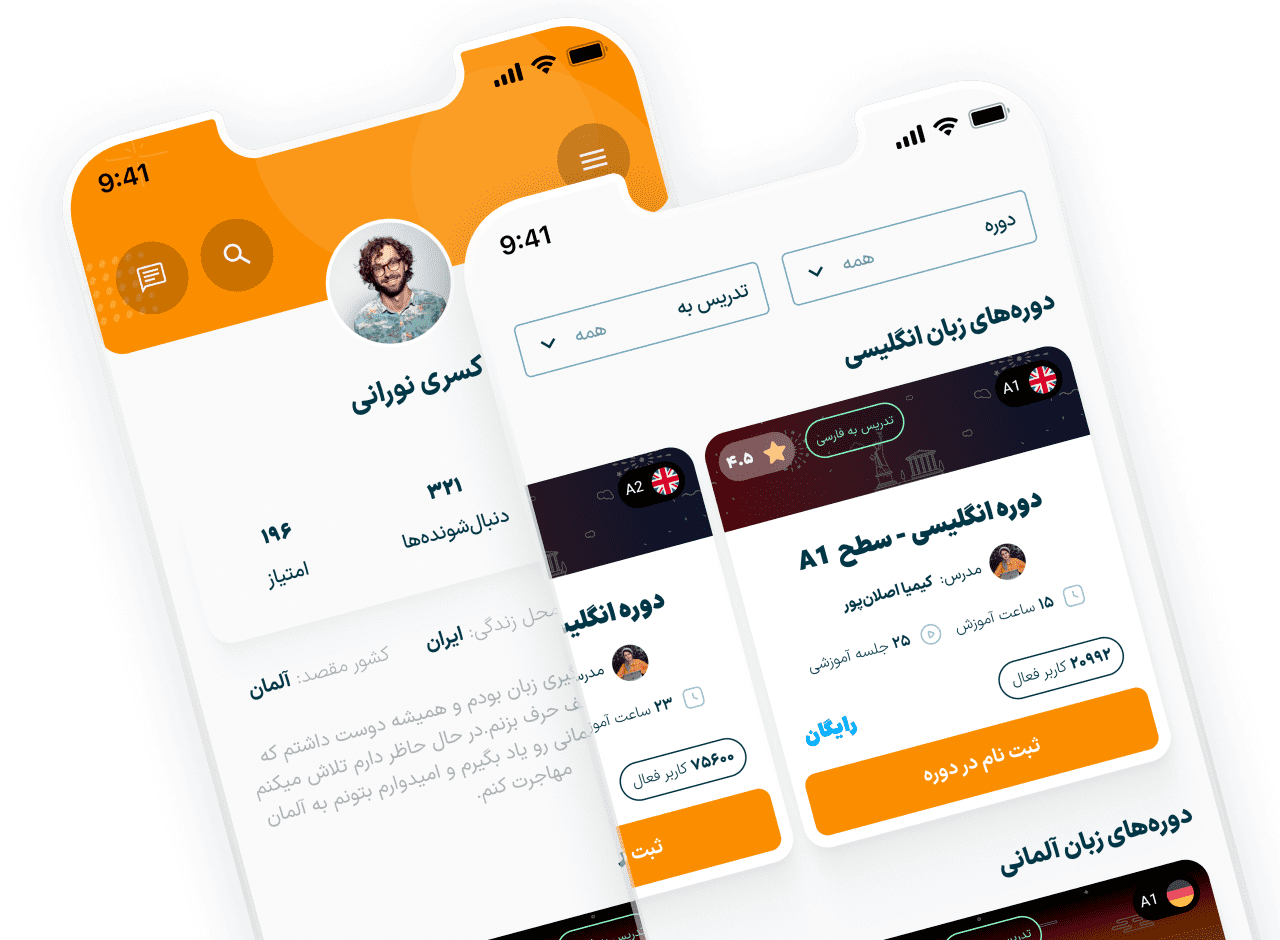
دوره :
مدرس :

زبان آموزش :

سطح آموزش :

تعداد درسها : درس
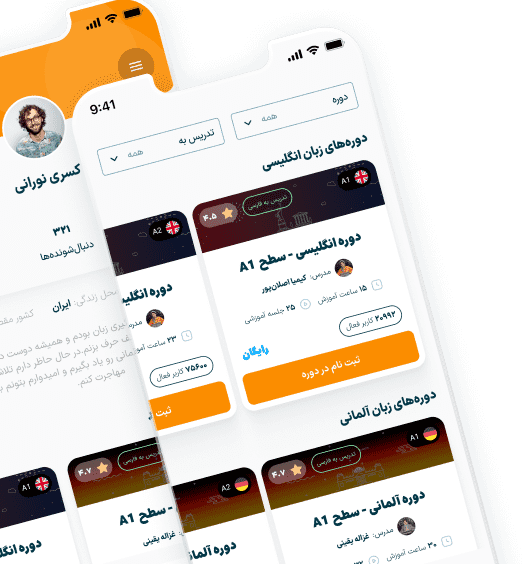
برای یادگیری و استفاده از آموزش ها اپلیکیشن GO2TRain را دانلود و از آن استفاده نمایید؛ دوره های خریداری شما از طریق اپلیکیشن در دسترس شما خواهد بود!
شما از اپلیکیشن GO2TRain می توانید برای آموزش و یادگیری استفاده کنید، دوره هایی هم که تهیه میکنید از طریق اپلیکیشن قابل دسترس هست اپلیکیشن هم راحت تره؛ هم سریع تر!


دیدگاه کاربران
دیدگاه
امتیاز